The Part A Deductible in 2023 saw an uptick, reflecting on everyone from individual beneficiaries to financial professionals advising them. With so many of us worried about healthcare, getting a grip on these changes doesn’t just help with future planning—it also means you or your clients can step into this space feeling sure and steady.
So, let’s jump right in and break down what this increase really means and how it shakes up the world of Medicare expenses for everyone involved. For anyone entangled in managing healthcare finances, whether for themselves or others, grasping these nuances could be the difference between stress and tranquility.
Understanding Medicare Part A Deductible in 2023
The Basics of Medicare Part A Deductible
The Medicare Part A deductible for 2023 was $1,600 per benefit period, which was a 3% increase from the 2022 deductible of $1,556. But what exactly is a benefit period?
A benefit period starts the day you’re admitted as an inpatient in a hospital or skilled nursing facility (SNF). It ends when you haven’t gotten any inpatient hospital or SNF care for 60 days in a row. You could have multiple benefit periods in a year, and you’d need to pay the Part A deductible for each one.
Comparing 2022 and 2023 Deductible Amounts
While the Part A deductible is rising, it’s not all bad news. Most Medicare beneficiaries saw a premium decrease in 2023. The standard monthly premium for Medicare Part B enrollees will be $164.90 for 2023, a decrease of $5.20 from $170.10 in 2022.
Here’s a quick comparison of the key Part A costs for 2022 and 2023:
| Cost | 2022 | 2023 |
|---|---|---|
| Inpatient hospital deductible | $1,556 | $1,600 |
| Daily coinsurance for 61st-90th Day | $389 | $400 |
| Daily coinsurance for lifetime reserve days | $778 | $800 |
| Skilled Nursing Facility coinsurance | $194.50 | $200.00 |
Factors Influencing the Annual Increase
So why does the Part A deductible keep rising? One key factor is that there’s no limit to the number of benefit periods a patient may experience in a year. The insurance company covering this risk has almost unlimited liability.
Increasing healthcare costs and an aging population also contribute to the annual hikes in Medicare costs. But there is some relief – the Medicare Savings Programs can help eligible low-income beneficiaries pay their premiums and other out-of-pocket costs.
Navigating Changes to Medicare Costs in 2023
Impact of Increased Costs on Beneficiaries
The rising Part A deductible can be a financial burden, especially for beneficiaries with multiple hospital stays in a year. In 2023, you paid $1,600 for each benefit period, which could have really added up.
But it’s not just the deductible – coinsurance amounts also increased. If you had a long hospital stay, you paid $400 coinsurance per day for days 61-90, up from $389 in 2022. For lifetime reserve days, the daily coinsurance was $800, up from $778.
Understanding the Role of Payroll Taxes in Funding Medicare
Did you know that payroll taxes largely fund Medicare Part A? Employees and employers each pay 1.45% of wages, while self-employed workers pay 2.9%.
These payroll taxes go into the Hospital Insurance Trust Fund, which pays for Medicare Part A benefits. Yet, as more people grow older and healthcare costs continue to climb, the trust fund is hitting a rough patch when it comes to staying solvent in the long run.
To shore up Medicare financing, some policymakers have proposed increasing the payroll tax rate, raising the taxable wage base, or using general revenues. But these solutions are often politically challenging.
Enrollment and Savings Opportunities for Medicare Beneficiaries
Maximizing Benefits During Open Enrollment Periods
Medicare Open Enrollment runs from October 15 to December 7 each year. During this time, beneficiaries can make changes to their coverage, such as:
- Switching from Original Medicare to a Medicare Advantage plan, or vice versa
- Changing Medicare Advantage plans
- Joining, dropping, or changing a Part D prescription drug plan
It’s important to review your coverage options each year, as your health needs and plan benefits can change. Look for plans that cover your preferred doctors, hospitals, and pharmacies, and compare costs like premiums, deductibles, and copayments.
Exploring Eligibility for Medicare Savings Programs
For low-income beneficiaries, Medicare Savings Programs can help pay premiums, deductibles, and other out-of-pocket costs. There are four programs, each with different eligibility criteria:
- Qualified Medicare Beneficiary (QMB) Program
- Specified Low-Income Medicare Beneficiary (SLMB) Program
- Qualifying Individual (QI) Program
- Qualified Disabled and Working Individuals (QDWI) Program
These programs are run by state Medicaid agencies, so eligibility and benefits vary by state. However, for those who make the cut, there’s a good chunk of financial help on the table. To see if you’re eligible, contact your state Medicaid office or fill out an online application.
Key Takeaway:
Medicare Part A deductible was $1,600 in 2023, a slight rise from 2022. Remember, each hospital stay starts a new benefit period with its own deductible. Good news? Medicare B premiums have dropped. Yet, healthcare costs keep climbing, pushing up deductibles and coinsurance rates.
Conclusion
So there you have it—the scoop on Part A deductible 2023 wrapped up neatly just for you. It’s not about fearing change; rather, it’s about knowing the lay of the land so well that when things shift under our feet—like they always do—we’re ready. We’ve looked at numbers hard enough to make our heads spin but came out smarter on the other side.
Remembering that every tweak in policy or adjustment amount holds power over real lives puts things into perspective. So let’s use this knowledge as both shield and compass as we chart through yet another year of navigating personal finance waters.
May your financial planning be robust and your stress levels low!
Streamlining the Medicare Surcharge Calculation Process.
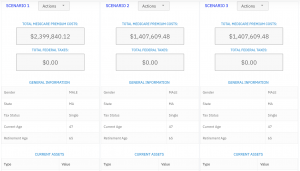
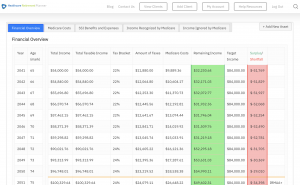
Our Healthcare Retirement Planner software is designed to streamline the retirement planning process for financial professionals. By providing an efficient way to calculate IRMAA costs, our tool helps you save time and focus on other aspects of your clients’ retirement plans.
- Faster calculations: Our software quickly calculates IRMAA costs based on your client’s income and tax filing status, eliminating manual calculations and potential errors.
- User-friendly interface: The intuitive design of our platform makes it easy for financial professionals to input data and generate results with minimal effort.
- Data integration: Seamlessly integrate our calculator into your existing financial planning tools or CRM systems for a more streamlined workflow.
- Easy to Understand Reports: Export reports to easily share with your clients
- Tax and Surcharge Modeling: see how different types of income affects both taxes and your surcharges.
In addition to simplifying the calculation process, using our Healthcare Retirement Planner can also help improve communication between you and your clients. With clear visuals that illustrate how IRMAA costs impact their overall retirement plan, you can effectively convey complex information in an easily digestible format. This enables clients to make informed decisions about their healthcare expenses during retirement while ensuring they are prepared for any potential changes in Medicare premiums due to income fluctuations. To learn more about how our software can benefit both you as a financial professional and your clients’ retirement planning experience, visit the features page. Streamlining retirement planning processes can help financial professionals save time and resources, allowing them to focus on other areas of their clients’ needs. Automated calculation of IRMAA costs is the next step in streamlining this process even further.