Ever felt like you’re trying to solve a complex puzzle with pieces that just don’t seem to fit? That’s what it can feel like navigating the labyrinth of Medicare Part B penalty waiver. Maybe you’ve heard whispers about late enrollment penalties, special circumstances, or even prescription drug coverage. But how does it all connect?
We get it – healthcare jargon isn’t exactly light reading material. It’s why we decided to roll up our sleeves and decode this Medicare mystery for you.
In the paragraphs ahead, we’ll untangle those puzzling terms and break down strategies on avoiding costly late fees. We’ll also dive into details about different health coverages interacting with Medicare Part B and demystify how premiums are calculated.
If deciphering Medicare feels like climbing Mount Everest without a map, consider this your Sherpa guiding the way…
Understanding Medicare Part B Penalty Waiver
The SEP, otherwise referred to as the Medicare Part B penalty waiver, provides an opportunity for those who have missed their Initial Enrollment Period. But what exactly is this penalty waiver and how does it work?
To start with, the Medicare Part B late enrollment penalty increases your monthly premium by an extra 10% for each full 12-month period you could have had coverage but didn’t sign up. That’s quite a hit. This makes understanding how to avoid these penalties essential.
What is Medicare Part B Penalty Waiver?
A little-known fact about late enrollment penalties is that they can be waived under certain circumstances through what’s called a Special Enrollment Period or SEP. The key here? Timely action.
If you’re eligible for an SEP, it means you’ve experienced specific life events such as leaving a job-based insurance plan or losing health coverage from your spouse’s current job – situations where people often delay enrollment into original medicare parts A and B.
Key Facts about Medicare Part B Penalty Waiver
Navigating healthcare can feel like trying to find your way in dense fog without any light source. However, some important facts will illuminate your path:
- You may qualify for an SEP if you lose employer coverage from either yourself or through your spouse’s employment.
- The appeal deadline after receiving the late-enrollment-penalty letter is 60 days – don’t miss out on that opportunity.
- Your benefits administrator at work plays a crucial role during this process – keep them informed so they can provide necessary documentation when needed.
With this information, the fog begins to lift and a clear path forward starts taking shape. Being aware of these key facts can be instrumental in helping you avoid that dreaded late enrollment penalty.
Medicare Part B Penalty Waiver Explained
The SEP gives you an eight-month period starting from when your employment or health plan coverage ends, allowing you to enroll without facing any penalties. This is where our metaphorical lifebuoy comes into play – clutch onto it.
Understanding the ins and outs of Medicare can be tricky. Let us assist you in your journey through the complexities of Medicare.
Key Takeaway:
Medicare Part B Penalty Waiver Insights: Missed your Initial Enrollment Period? No worries. The Medicare Part B penalty waiver or Special Enrollment Period (SEP) is here to save the day. This lifesaver waives late enrollment penalties under specific circumstances like losing job-based insurance. Remember, it’s crucial to act quickly and always keep your benefits administrator updated about any changes in your situation.
Late Enrollment and Enrollment Penalties in Medicare
When it comes to enrolling in Medicare, timing matters. Late enrollment can lead to increased premiums or penalties that could affect your health coverage.
Understanding the Impact of Late Enrollment
If you miss your initial enrollment period for Part B when first eligible, a late enrollment penalty might apply. The penalty increases the monthly premium by an extra 10% for each full 12-month period you were eligible but didn’t enroll. Here’s where to get started with Medicare.
This isn’t a one-time fee but rather something that stays with you as long as you have Part B – not quite what anyone wants from their golden years. Imagine getting socked with a higher premium every month just because you missed the sign-up deadline.
You might be thinking: “I’ll just wait until I need healthcare before signing up.” But beware. This strategy is akin to waiting until after your house burns down to buy home insurance. By then, it’s too late, and you’re stuck paying out-of-pocket costs.
The Costly Consequences of Delaying Your Decision
The reality is stark: delaying this decision may cost more than just money; It could jeopardize access to critical health care services when needed most.
Avoid being penny wise and pound foolish. Don’t delay your enrollment into Part A or Part B during the initial enrollment period unless qualified for special circumstances like having job-based insurance through current employment. Check if you qualify for premium-free Part A.
Also, consider this: The penalty for Part A increases the monthly premium by 10% for each year you didn’t sign up. It’s a bitter pill to swallow.
Avoiding the Pitfalls of Late Enrollment
The silver lining is that with mindful organization and opportune choices, these charges can be evaded. Understanding your Medicare options and enrolling at the right time can save both money and headaches down the line. Get started today.
Key Takeaway:
Timing is crucial when enrolling in Medicare to avoid increased premiums or penalties. Late enrollment for Part B can lead to a permanent monthly penalty. Delaying your decision might cost more than just money; it could limit access to critical healthcare services. But, with careful planning and timely action, you can dodge these pitfalls.
Navigating through Different Medicare Part B Enrollment Periods
Medicare Part B, covering outpatient services and preventive care, has distinct enrollment periods. Let’s shed light on these critical timelines to help you avoid late enrollment penalties.
The Initial Enrollment Period (IEP)
Your first chance to join Medicare is during the IEP, which starts three months before your 65th birthday month and extends for seven months. It’s a good idea to sign up even if you still have health coverage from an employer or spouse’s current job because delaying could result in higher premiums due to late fees.
The Special Enrollment Period (SEP)
If you’re covered under a group insurance plan based on current employment, either yours or that of your spouse’s, the SEP lets you enroll in Medicare without penalty for up to eight months after the employment ends or when the employer coverage ends. But be careful. Not all types of coverage count as creditable – retiree plans don’t offer this grace period.
The General Enrollment Period (GEP)
If both initial and special periods are missed, GEP becomes relevant – it runs from January 1st through March 31st each year with benefits starting July 1st. Get started with Medicare details more about these dates.
Bear in mind that failing timely registration can lead to lifelong monthly premium increases due ‘late enrollment penalties’. For example: A delay beyond one full year will add another 10% onto your standard premium.
In certain circumstances though there may be options available such as requesting a ‘penalty waiver’ – but this is not a guarantee and has strict rules attached. To understand your options, it’s advisable to request for reconsideration with the Social Security Administration within 60 days of receiving the penalty letter.
Avoiding late enrollment penalties might seem complex, but knowing these key timelines makes navigating Medicare Part B much easier.
Key Takeaway:
Getting a grip on Medicare Part B’s enrollment periods can keep you safe from late penalties. Your first opportunity is the Initial Enrollment Period, which comes around your 65th birthday. There are also Special Enrollment Periods for folks who already have coverage. But watch out – not all plans make the cut. If you’ve missed both of these windows, don’t worry. You still have the General Enrollment period that happens every year to count on. Just remember, putting off enrolling could hike up your premiums; if you’re stuck in a jam because of this, it’s worth looking into how to dodge penalty costs.
How Health Coverage Interacts with Medicare Part B
It’s essential to be aware of how health coverage from a job ties in with Medicare Part B if you’re currently employed. If your employer has 20 or more employees, typically the group insurance from work will be the primary payer. However, for smaller employers, Medicare may take precedence.
Your current job-based insurance might also affect when you decide to join Medicare. It’s crucial to understand this interaction because late enrollment penalties can increase monthly premiums by an extra 10% each year if not managed properly.
Employer Health Plans & Retiree Coverage Considerations
A key aspect of managing potential penalties involves understanding when your employer coverage ends. This is because once employment ends or health coverage lapses, you’ll usually have an eight-month period (known as a special enrollment period) to sign up for Medicare without facing any late fees.
The question then arises: “Do I qualify for premium-free part A?” which depends on factors like age and work history. You can find detailed eligibility criteria here.
In case of retiree plans or COBRA coverage post-employment; these do not count as active employer health coverages in terms of avoiding medicare late enrollment penalties so tread carefully.
Health Coverage Options with Medicare Part B
Different types of private insurances such as Medigap policies help fill gaps in Original Medicare services but they function differently. They can’t be used to pay for Medicare premiums and generally don’t work with any other type of health coverage such as employer plans or Veterans Affairs benefits.
Medicare Advantage Plans present an alternate option for acquiring Original Medicare benefits, but they come with their own regulations concerning expenses and network limitations that must be taken into consideration when weighing healthcare selections.
Key Takeaway:
Knowing how your job’s health plan interacts with Medicare Part B can save you from hefty late fees. If you leave your job, remember the eight-month special enrollment period to join Medicare penalty-free. But be cautious: retiree or COBRA coverage doesn’t count as active employer health insurance against these penalties.
Private insurances, such as Medigap, play a critical role in providing additional coverage to help fill the gaps left by Medicare. This is essential for many individuals who need more comprehensive healthcare protection.
Prescription Drug Coverage under Medicare Part B
Medicare Part B is often seen as the ticket to comprehensive health care, but it’s crucial to understand how it intertwines with prescription drug coverage. By grasping this link, you can make more informed decisions about your healthcare.
Evaluating Different Prescription Drug Plan Options
The landscape of prescription drug plans within Medicare Part B might seem complex at first glance. But don’t worry. We’re here to help navigate these waters. When evaluating different plan options, consider both the breadth of coverage and cost.
In general, most drugs administered in a doctor’s office or other outpatient settings come under Part B’s umbrella. This includes certain vaccines and injections needed for treatment or prevention of illness.
If you didn’t join a Medicare drug plan when first eligible though, there may be penalties involved which increase your premium by 1% for each month delayed up until a maximum penalty of 12% per year. That’s why understanding all facets before making any decision becomes vital.
Navigating Late Enrollment Penalties
Late enrollment in Part D could result in increased costs down the line – an extra burden nobody wants on their shoulders. A late enrollment penalty applies if you go without creditable prescription drug coverage (from either Medicare or another source) for any continuous period that exceeds 63 days after your Initial Enrollment Period ends.
This can certainly feel like navigating through stormy weather but remember: knowledge is power. The right information will guide you safely into port – ensuring no unexpected penalties darken your horizon.
Promoting Informed Decisions
Gaining an understanding of the intricacies associated with Medicare Part B prescription drug coverage is like solving a complex puzzle. But, with every piece you place, the image becomes clearer and more understandable.
Gathering the necessary information to make an informed decision is essential, so don’t be afraid to ask questions and seek out answers. And remember – asking questions is not only okay; it’s encouraged.
Key Takeaway:
Get the Know-How: Medicare Part B intertwines with prescription drug coverage, so understanding this link lets you make savvy healthcare choices. It’s a complex landscape but fear not – we’re here to guide. Watch out for late enrollment penalties in Part D and remember, knowledge is power. Each piece of information you gather fits into the puzzle, making your path towards informed health decisions clearer.
Special Circumstances and Considerations in Medicare Part B
Medicare Part B offers vital health coverage, but life isn’t always straightforward. There are special circumstances to consider when dealing with enrollment and avoiding penalties.
Social Security Disability Benefits & Employment
When receiving Social Security disability benefits, it is essential to be aware of how this affects your Medicare coverage; especially as automatic enrollment into Parts A and B occurs after 24 months, potentially leading to late enrollment penalties if not managed correctly. Typically, after 24 months of getting these benefits, you automatically get enrolled into Parts A and B.
This means if you’re still working or have job-based insurance from a spouse’s current job during that period, there could be implications for late enrollment penalties if not handled correctly.
Job Changes & Health Coverage Transitions
A change in employment status can affect your decision about when to join Medicare. For example, if employer coverage ends because of retirement or job loss before reaching 65 years old – the age at which most people start their Medicare – then understanding your options is crucial to avoid a higher premium due to late fees.
You may qualify for a Special Enrollment Period (SEP) depending on specific conditions such as changes in employer plan members or retiree plan offerings. It allows you eight months after employment ends or group insurance terminates – whichever happens first -to sign up without facing any penalty. SSA’s request for reconsideration form can also help contest unfair charges related directly to unique situations like these.
Creditable Prescription Drug Coverage
In addition to health care services under Part B, prescription drug coverage is another critical aspect where timing matters. If there was creditable drug coverage from another source like an employer’s health plan before joining part D, it can help avoid late enrollment penalties.
But remember, being eligible for a Medicare Savings Program (MSP) could potentially eliminate the Part B late enrollment penalty altogether. MSPs, provided by states, are accessible to people with incomes below a certain limit and aid in paying Medicare expenses like premiums, deductibles, and co-insurance.
Key Takeaway:
Medicare Part B enrollment can be a maze of special circumstances and penalties. If you’re on Social Security disability benefits, know that after 24 months, you’ll automatically join Parts A and B. Changes in employment or health coverage might mean considering your options to avoid higher premiums due to late fees. If the Special Enrollment Period (SEP) applies to your situation, make sure to use it as an opportunity for avoiding any potential hiccups with late enrollment.
Avoiding Late Enrollment Penalties in Medicare Part B
Medicare part b, just like a good buddy, is always there for you. But missing your enrollment period can be as annoying as forgetting to pick up your best friend from the airport.
If you delay enrolling into Medicare Part B beyond your initial enrollment period without having creditable coverage elsewhere, it’s likely that you’ll face late enrollment penalties. So how do we avoid this?
Tips for Timely Enrollment
The first step towards avoiding late fees involves understanding the key periods of Medicare part b – Initial Enrollment Period (IEP), Special Enrollment Period (SEP) and General Enrollment Period (GEP). For most people turning 65, their IEP starts three months before their birth month and ends three months after.
In case you missed it or decided not to join during IEP because you were still working and had employer health insurance through either yours or spouse’s current job; SEP becomes relevant. The special enrollment lasts eight-months starting from when employment ends or employer coverage ends, whichever comes first.
Navigating Coverage Options
To stay clear of any higher premium due to a penalty waiver, consider these options:
- You could continue with an existing group insurance plan if eligible,
- Switch over to retiree coverage if available,
- Or enroll into Medicare right away once eligibility kicks in at age 65. But what happens if circumstances change? You might wonder.
Changes In Health Care Needs & Circumstances
Say hello again. It’s no secret life changes are inevitable but luckily so does the opportunity to adjust plans during annual open-enrollment periods allowing us all more flexibility.
And, if you have limited income and resources, the Medicare Savings Program (MSP) might help pay Part B premiums too.
Let’s be clear, not enrolling on time could mean leaving money untouched – that’s never wise. For more info on your enrollment options and how to dodge penalties, check this out:
Key Takeaway:
Medicare Part B is like a dependable friend, but missing your sign-up window can cause headaches. To dodge late fees, know the key enrollment periods: Initial (IEP), Special (SEP) and General (GEP). Consider sticking with group insurance, switching to retiree coverage or jumping into Medicare at 65. Remember – life changes are expected and so it’s important to adjust your healthcare plan accordingly to stay covered.
In-depth Analysis of Medicare Part B Premiums
Let’s start with a quick fact: the Part B late enrollment penalty is 10%. This might seem steep, but understanding how these premiums are calculated can help you plan better.
The calculation involves two factors – the standard monthly premium and your income. The standard monthly premium, which changes every year, serves as a base for all enrollees. For instance, in 2023 it was $148.50.
Your income, on the other hand, plays a crucial role in determining if you’ll pay more than this amount or not. If your modified adjusted gross income (MAGI) is above certain thresholds set by Medicare each year – brace yourself for an Income-Related Monthly Adjustment Amount (IRMAA).
Analyzing IRMAA & Its Impact on Your Premiums
You may wonder what this so-called “IRMAA” is about? Well, it’s basically an extra charge added to your Part B premium if your MAGI exceeds specific limits established by Medicare annually.
This charge isn’t random though; there’s method behind its madness. It follows tiered brackets where higher incomes get charged more than lower ones – much like tax brackets do.
Avoiding Penalties With Timely Enrollment
If penalties sound intimidating – don’t fret. You can avoid them entirely with timely enrollment during the Initial Enrollment Period that begins three months before turning 65 and ends three months after reaching the age milestone.
FAQs in Relation to Medicare Part B Penalty Waiver
Can Medicare penalties be waived?
Yes, under certain conditions. You might qualify for a penalty waiver if you were misinformed about the need to enroll in Part B.
What are exceptions to Medicare Part B late enrollment penalty?
You may avoid the penalty if you had health coverage from an employer or union when you first became eligible for Medicare.
Can I stop Medicare Part B without penalty?
Absolutely. If your situation changes and you no longer need Part B, it’s possible to drop it during specific periods without facing any penalties.
Can I cancel Medicare Part B if I have other insurance?
Sure can. If your current health coverage meets certain requirements, like being from an employer with over 20 employees, cancelling part b is allowed.
Conclusion
Decoding the ‘Medicare Part B penalty waiver’ doesn’t have to feel like an uphill battle. With a clear understanding, you can navigate enrollment periods and avoid late fees.
Remember, health coverage options interact differently with Medicare Part B. So it’s crucial to weigh these factors when choosing your plan.
Your premiums are calculated based on various elements including standard monthly costs and income-related adjustments. Being aware of this helps prevent unpleasant surprises down the line.
And let’s not forget prescription drug plans – knowing your options here is key for comprehensive coverage. Stay informed, stay prepared!
Table of Contents:
- Understanding Medicare Part B Penalty Waiver
- Late Enrollment and Enrollment Penalties in Medicare
- Navigating through Different Medicare Part B Enrollment Periods
- How Health Coverage Interacts with Medicare Part B
- Prescription Drug Coverage under Medicare Part B
- Special Circumstances and Considerations in Medicare Part B
- Avoiding Late Enrollment Penalties in Medicare Part B
- In-depth Analysis of Medicare Part B Premiums
- FAQs in Relation to Medicare Part B Penalty Waiver
- Conclusion
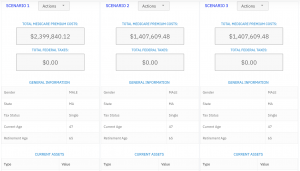
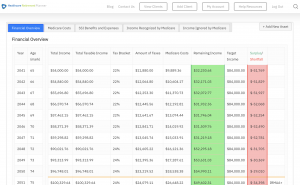
Streamlining the Medicare Surcharge Calculation Process.
Our Healthcare Retirement Planner software is designed to streamline the retirement planning process for financial professionals. By providing an efficient way to calculate IRMAA costs, our tool helps you save time and focus on other aspects of your clients’ retirement plans.
- Faster calculations: Our software quickly calculates IRMAA costs based on your client’s income and tax filing status, eliminating manual calculations and potential errors.
- User-friendly interface: The intuitive design of our platform makes it easy for financial professionals to input data and generate results with minimal effort.
- Data integration: Seamlessly integrate our calculator into your existing financial planning tools or CRM systems for a more streamlined workflow.
- Easy to Understand Reports: Export reports to easily share with your clients
- Tax and Surcharge Modeling: see how different types of income affects both taxes and your surcharges.
In addition to simplifying the calculation process, using our Healthcare Retirement Planner can also help improve communication between you and your clients. With clear visuals that illustrate how IRMAA costs impact their overall retirement plan, you can effectively convey complex information in an easily digestible format. This enables clients to make informed decisions about their healthcare expenses during retirement while ensuring they are prepared for any potential changes in Medicare premiums due to income fluctuations. To learn more about how our software can benefit both you as a financial professional and your clients’ retirement planning experience, visit the features page. Streamlining retirement planning processes can help financial professionals save time and resources, allowing them to focus on other areas of their clients’ needs. Automated calculation of IRMAA costs is the next step in streamlining this process even further.